Health and Social Care
Women’s Health Champion Spring 2025 update
May 12, 2025 by Professor Anna Glasier No Comments | Category Women's Health Champion
It is now a little over two years since I became Women’s Health Champion and I think I am at last getting the hang of how to do the job. There has been a lot going on since I wrote my last blog, quite a bit of it has involved seeking your views on what Phase 2 of the Women’s Health Plan should look like, but there has been progress in other areas too. Looking back at the priorities of the first phase of the plan, from my perspective we seem to have done a fair amount.
Menopause and menstrual health
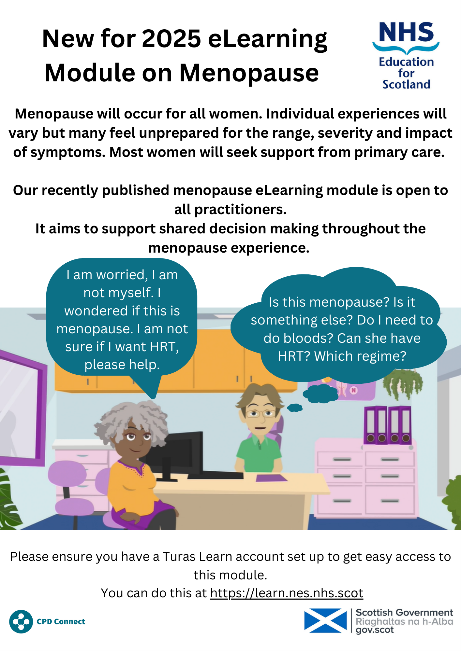
I think we have done well on opportunities for better informing the public about both menopause and menstrual health. I hope there are now far fewer people in Scotland today for whom the menopause is a well-kept secret. There are many articles and features about the menopause in both the print and broadcast media. Menstrual health too is rapidly becoming less stigmatised, I noticed a strong message – emblazoned around the perimeter of the Emirates Stadium during a televised men’s premier league match (Arsenal v Chelsea) – about girls being reluctant to play football because they are worried about ‘period leaks’. I believe women are gradually becoming better informed about what is normal during menstruation and menopause, and when something is not normal are taking steps to seek help. But seeking help remains challenging. We hear repeatedly that women don’t feel listened to when talking to health care professionals about menstrual health, young people report particularly that they are told that heavy, painful periods are normal in adolescence and that they will grow out of them. For many this is true, but the problem still leads to girls missing school and sharing simple advice about how to manage troublesome menstruation is not difficult. The recently launched NES e-learning modules on menopause and menstrual health should help healthcare professionals to give better advice and to feel confident in managing these extremely common problems. The feedback about the modules has been excellent and I encourage everyone working in the NHS to have a look at them.
Waiting times for gynaecology
As well-informed as women and healthcare professionals might be about gynaecological conditions, if the waiting times for an outpatient appointment and surgery, if required, are very long then neither the patient nor the healthcare professional are going to be satisfied.
Recognising that waiting times for gynae across Scotland are unacceptable, I have been working with Ministers and colleagues across the Scottish Government, the Centre for Sustainable Delivery and NHS Boards themselves to discuss solutions.
For me this should involve some radical thinking about how gynaecology services should be delivered. When I trained in gynaecology it was a surgical specialty and each year we did thousands of laparoscopic sterilisations, thousands of D and C’s and thousands of surgical abortions. D and C has been replaced by endometrial biopsy done in the clinic, over 93% of abortions in Scotland are now done medically and few women are sterilised. Medical treatments for heavy menstrual bleeding, endometriosis, fibroids are much more effective than they were 30 years ago and probably fewer than 25% of women seen in gynae out-patients departments end up needing surgery. A radical solution to the gynaecology waiting times is a priority for me in the next year and, in time, personally I would like to see an enhanced role for Sexual and Reproductive Health (SRH) services incorporating what in Europe is called Community or Office Gynaecology.
Mental Health
Waiting a long time to have gynaecology problem sorted has a detrimental effect on women’s mental health. In the first phase of the plan a short piece on mental health was included in the section on the Strategic Context. It acknowledged the importance of mental health, and the specific mental health challenges faced by women and recognised the key importance of mental wellbeing in overall health. In our discussions with our networks and various stakeholder groups the need to include mental health in Phase Two of the Plan has been frequently raised. I recently attended a fascinating meeting at the Royal College of Physicians of Edinburgh entitled Breaking the Silence – Exploring the Stigma of Women’s Mental Health. Three female psychiatrists discussed the issue, and we have since met with one of them to discuss what more we could be doing to support women’s health as we continue our discussions about Phase Two of the Plan.
Abortion and contraception
The Expert Group reviewing the law on abortion has met eight times and we are now finalising the recommendations that we should like to make to Scottish Ministers. There will hopefully be a public consultation once we publish our final report, once Ministers have considered our recommendations. When we do have a public consultation, it would be helpful if as many of you as possible weigh in with your opinions so that we get a balance of views.
We still have not solved the problem of reduced access to long-acting reversible contraception (LARC) despite lengthy discussions. We have explored all the options for ways to deliver LARC services and I will be speaking to the Boards in soon about possible solutions to this.
We are still grappling – at a UK level – with what we should be doing, indeed could possibly do, about declining use of hormonal contraception, which I think is contributing to rising abortion rates. This will be a hard nut to crack as it is a reflection of societal changes and is likely to have other long-term consequences since we know that use of hormonal contraception provides significant protection against endometrial, ovarian and colon cancer. Endometrial cancer is already increasing likely due to rising levels of obesity, but the picture will get worse if there is wholescale abandonment of the pill.
In March, I attended the third Scottish Post-partum Contraception conference. A lot of good work has been done preparing eye-catching information materials for women on their options (available on NHS Inform) and a national training and accreditation system is in place throughout Scotland. However, in some parts of Scotland fewer than 20% of women recall having been given any advice about postpartum contraception during their pregnancy. Although many midwives are enthusiastic about immediate post-placental insertion of an IUD in order to happen routinely it must be included as a core part of the UK Royal College of Midwives training curriculum. Likewise, it should be part of the curriculum for training obstetricians. It is obvious that the person who is best placed to insert a post-partum IUS is the person who delivers the baby regardless of who that is and of the mode of delivery.
Eliminating Cervical Cancer
The core Expert Group on Eliminating Cervical Cancer, together with the three subgroups (on HPV vaccination, screening and treatment) are continuing to meet regularly to develop and refine recommendations on how Scotland will progress towards cervical cancer elimination. We know that we need to increase the uptake of vaccination and screening, particularly in the most deprived areas of Scotland but the downward trends we have seen in recent years seem to be a result of societal changes and not failings in service delivery. That of course makes it challenging to forecast how successful the recommended interventions will be, thereby complicating the process of setting a date for elimination, even if other countries have been tempted into doing so. Perhaps they are less pessimistic about the vagaries of human behaviour.
Optimising Future Health
Following a number of meetings to discuss Phase Two of the Women’s Health Pan, early discussions have highlighted Optimising Future Health as a potential area of focus.
There are many things we can all do to support our long-term health at any age which will help prevent some health concerns in later life. Although, we know we need to do more in the next phase for post-menopausal women, potentially including pelvic and bone health. With the Health and Social Care Alliance I participated in a webinar on the subject which was extremely well received. You can watch it on the Alliance website and I thoroughly recommend it, especially the first half, you can stop watching when I appear!
I have a personal interest in the subject of bone health. I visited Dr Maria Talla at the Golden Jubilee Hospital at the beginning of February. Dr Talla is an endocrinologist with an interest in bone health who has set up a sophisticated IT fracture liaison service which detects many more people at risk of osteoporosis than the laborious ‘doing it by hand’ systems and could predict and therefore prevent many osteoporotic fractures throughout Scotland, reducing much morbidity and saving a lot of money. I hope to be able to do a bit to help Dr Talla make the case for rolling the FLS digital system out nationally.
Earlier this year, I had the privilege of being interviewed by the Scottish Teaching Union NASUWT to talk about my role as Women’s Health Champion and discuss women’s health in the education sector. You can listen to this podcast interview here: Prof Glasier on Women’s Health | A Better Deal For Scotland’s Teachers.
Finally, don’t forget to join the Women’s Health Champion Seminar series. The next seminar will be on take place on Thursday 5th June. In this seminar we will hear from Dr Emma Slaymaker from the London School of Hygiene and Tropical Medicine who will tell us about some research that she plans to do on falling birth rates in the UK.
That is probably enough from me for now, I still think that being Women’s Health Champion is possibly one of the best jobs in the world and I am still extremely honoured to have the role.

Leave a comment
You must be logged in to post a comment.